Focus on Pancreatic Cancer: Early Detection and Timely Treatment
The Pancreas: The Core of Digestion and Metabolism
The pancreas,is an essential gland in vertebrates with both exocrine and endocrine functions. It plays a critical role in human digestion and metabolism.

1. Exocrine Function
The exocrine portion of the pancreas is primarily composed of acini and ducts connecting to the intestinal cavity. It is responsible for secreting various digestive enzymes and bicarbonate, which together form pancreatic juice. This juice enters the duodenum and helps digest carbohydrates, fats, and proteins, making it a crucial digestive fluid. Each day, pancreatic acini produce approximately 1200 to 1500 milliliters of pancreatic juice, which contains the following components:
Digestive Enzymes: Including amylase, lipase, trypsin, chymotrypsin, and nuclease, which break down proteins, carbohydrates, fats, and nucleic acids.
Bicarbonate: A mildly alkaline substance that neutralizes stomach acid and protects the intestinal lining.
2. Endocrine Function
The endocrine portion of the pancreas consists of the islets of Langerhans. An adult has about 1 to 2 million islets scattered among the acini. The islets have no ducts but are richly supplied with capillaries, allowing each islet cell to contact the blood supply. The islet cells are of various types, mainly including:
Alpha Cells: Secrete glucagon, which promotes glycogen breakdown in the liver, thereby raising blood sugar levels.
Beta Cells: Secrete insulin, which lowers blood sugar and promotes glycogen synthesis in the liver.
3. Blood Sugar Regulation Mechanism
Insulin and glucagon work together through a feedback mechanism to regulate blood sugar levels. If insulin secretion is insufficient, either absolutely or relatively, it can lead to diabetes.
4. Structure of the Pancreas
The pancreas is a long, flat gland located behind the stomach. Its structure primarily includes:

1. Head of the pancreas 2. Uncinate process
3. Pancreatic notch 4. Body of the pancreas
5. Anterior surface 6. Inferior surface
7. Superior margin 8. Anterior margin
9. Inferior margin 10. Omental tuberosity
11. Tail of the pancreas 12. Duodenum
Pancreatic Cancer: The "Silent Killer"
Pancreatic cancer refers to malignant tumors that originate in the pancreas. The most common type is pancreatic adenocarcinoma, accounting for over 85% of cases. Due to its subtle early symptoms, pancreatic cancer is often not detected until it has reached an advanced stage, making treatment challenging and prognosis poor.
Common Symptoms: Don't Ignore Them
l Jaundice: Yellowing of the skin and eyes, often accompanied by dark urine.
l Abdominal and Back Pain: Particularly around the stomach or back, with pain typically worsening over time.
l Unexplained Weight Loss: Often accompanied by loss of appetite and indigestion.
l Gastrointestinal Symptoms: Nausea, vomiting, and steatorrhea (fatty stools).
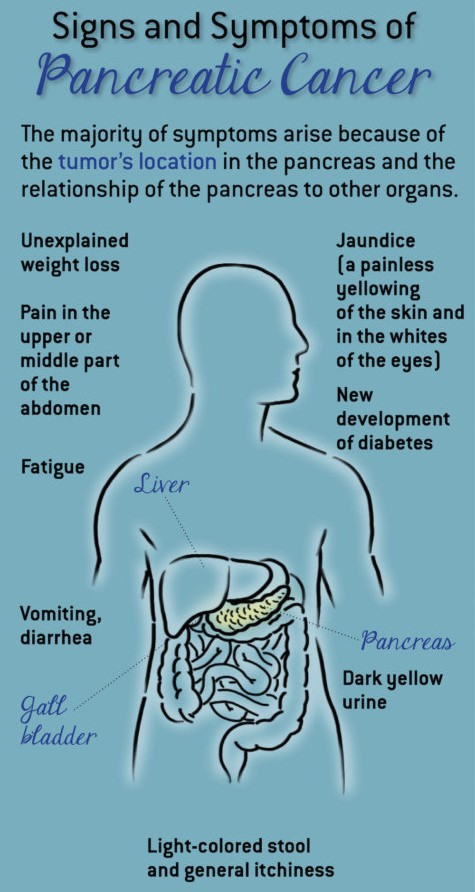
These symptoms usually appear only after the cancer has spread, making early attention to bodily changes essential.
High-Risk Groups: Factors That Increase the Risk
Risk factors for pancreatic cancer include smoking, obesity, diabetes, and family history. Smoking is currently the most significant known modifiable risk factor, with long-term smokers being about twice as likely to develop pancreatic cancer compared to non-smokers.
Early Screening: The Key to Improving Survival Rates
Although early diagnosis of pancreatic cancer is challenging, regular check-ups and early screening are crucial for high-risk individuals. Through medical imaging, blood tests, and professional medical judgment, early-stage intervention can improve patient survival rates. Here are some blood tests related to pancreatic cancer:
1. Carcinoembryonic Antigen (CEA)
CEA is a protein often used as a tumor marker. While it is not specific to pancreatic cancer, elevated levels in some patients may indicate the presence of the disease. However, elevated CEA levels can also be associated with other types of cancer or non-cancerous conditions.
2. Carbohydrate Antigen 19-9 (CA 19-9)
CA 19-9 is a tumor marker commonly associated with pancreatic cancer. It is one of the most frequently used blood markers for pancreatic cancer detection. Elevated CA 19-9 levels may suggest pancreatic cancer, particularly in the diagnosis and treatment process. However, not all pancreatic cancer patients will have elevated CA 19-9, and the marker may be ineffective for some.
3. Insulin and Insulin-Like Growth Factor (IGF)
Abnormal levels of insulin and IGF-1 (Insulin-Like Growth Factor 1) may be related to pancreatic dysfunction and certain types of cancer. Although insulin and IGF-1 are not typically used for initial pancreatic cancer screening, they can provide additional information about pancreatic function and potential abnormalities.
4. Blood Glucose Levels
Pancreatic cancer may lead to abnormal blood sugar levels, such as the development of diabetes. Glycated hemoglobin (HbA1c) is a product of glucose binding to hemoglobin in red blood cells and is typically used as a reference standard for average plasma glucose concentration over time. It is used as a diagnostic test for diabetes and as an assessment test for blood sugar control in diabetic patients.
Healthy Lifestyle: Reducing the Risk of Disease
Avoiding smoking, maintaining a healthy weight, and adopting a balanced diet are effective measures to reduce the risk of pancreatic cancer. Non-smokers and those who limit red or processed meat consumption have a relatively lower risk of developing pancreatic cancer.
Conclusion
Pancreatic cancer is a silent and deadly disease, but we can reduce its risk by staying vigilant, undergoing timely screenings, and adopting a healthy lifestyle. Let's all focus on pancreatic cancer and protect our health!

















